Psychiatry Soap Note Template
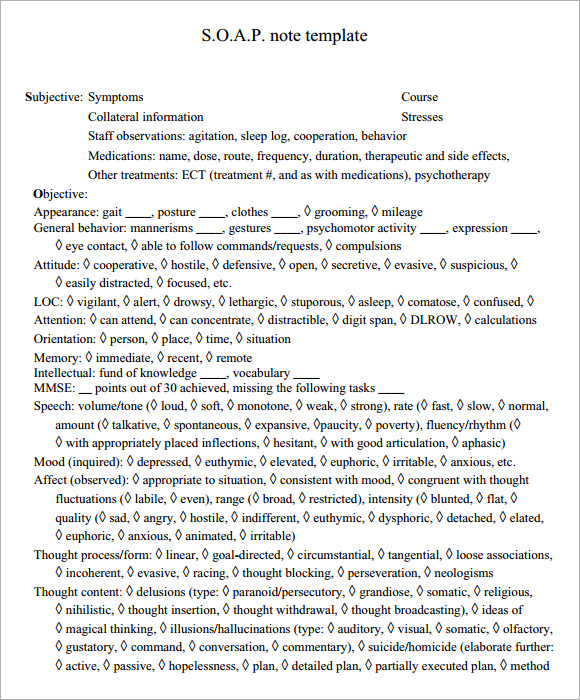
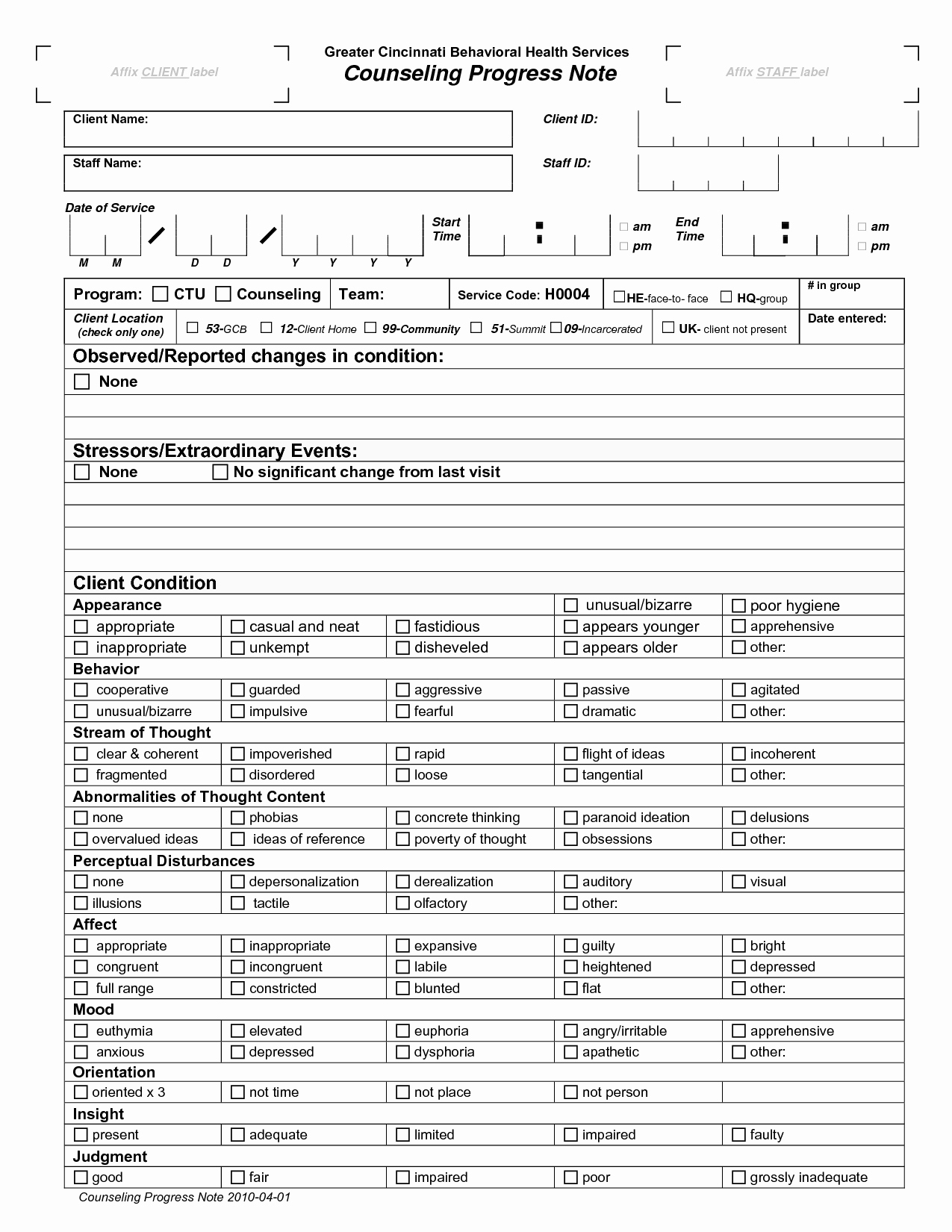
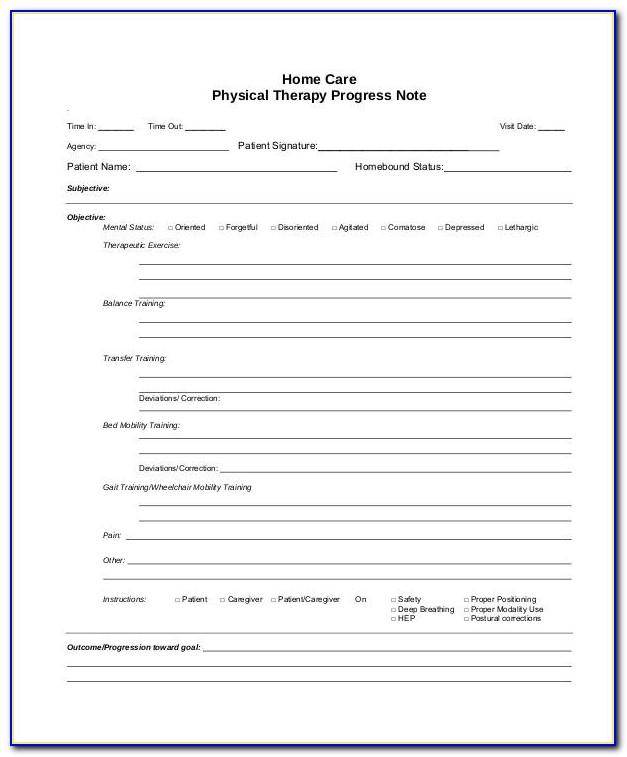
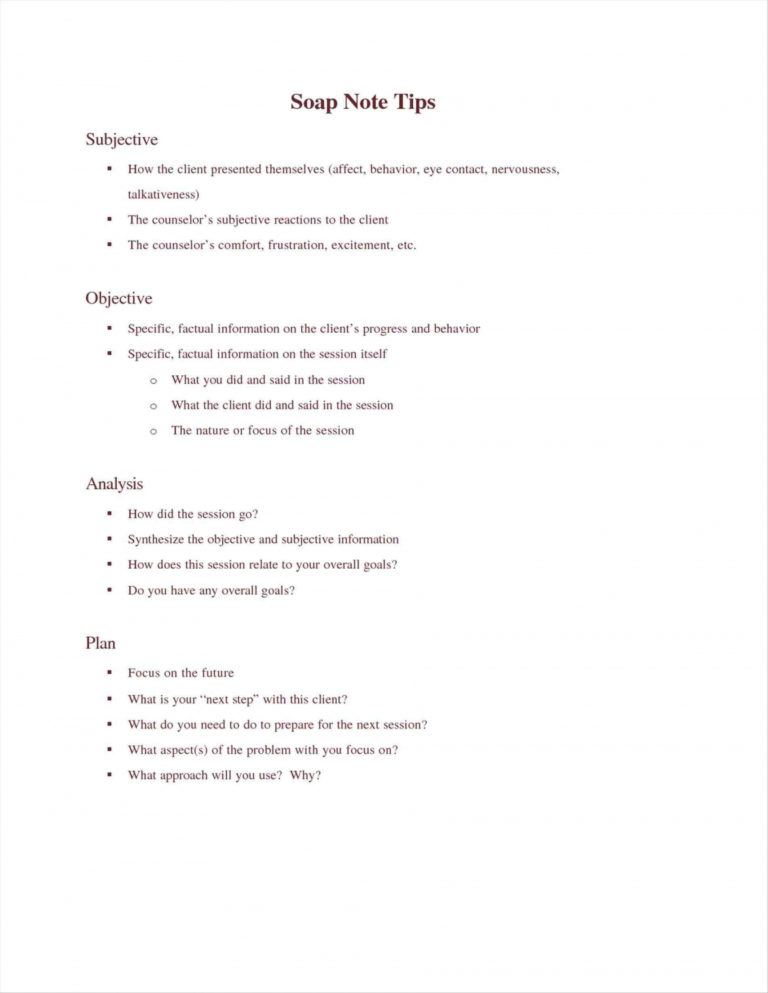
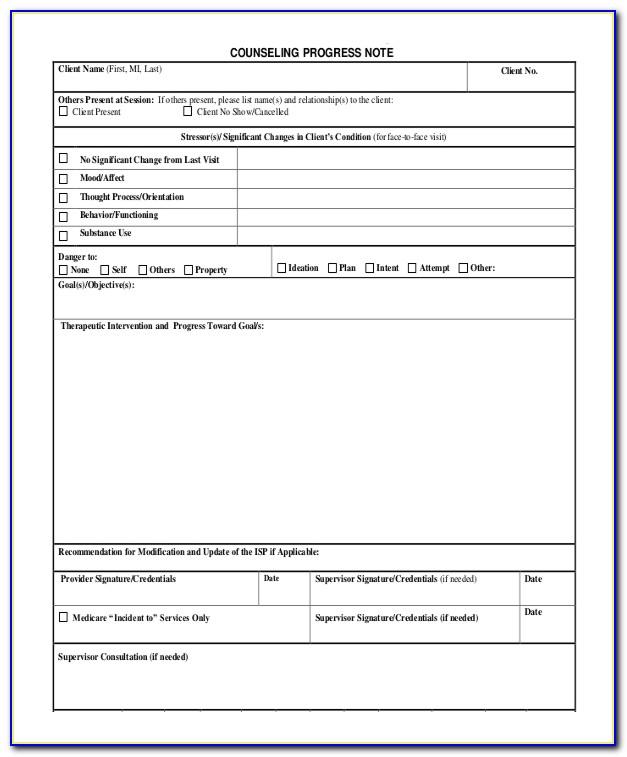
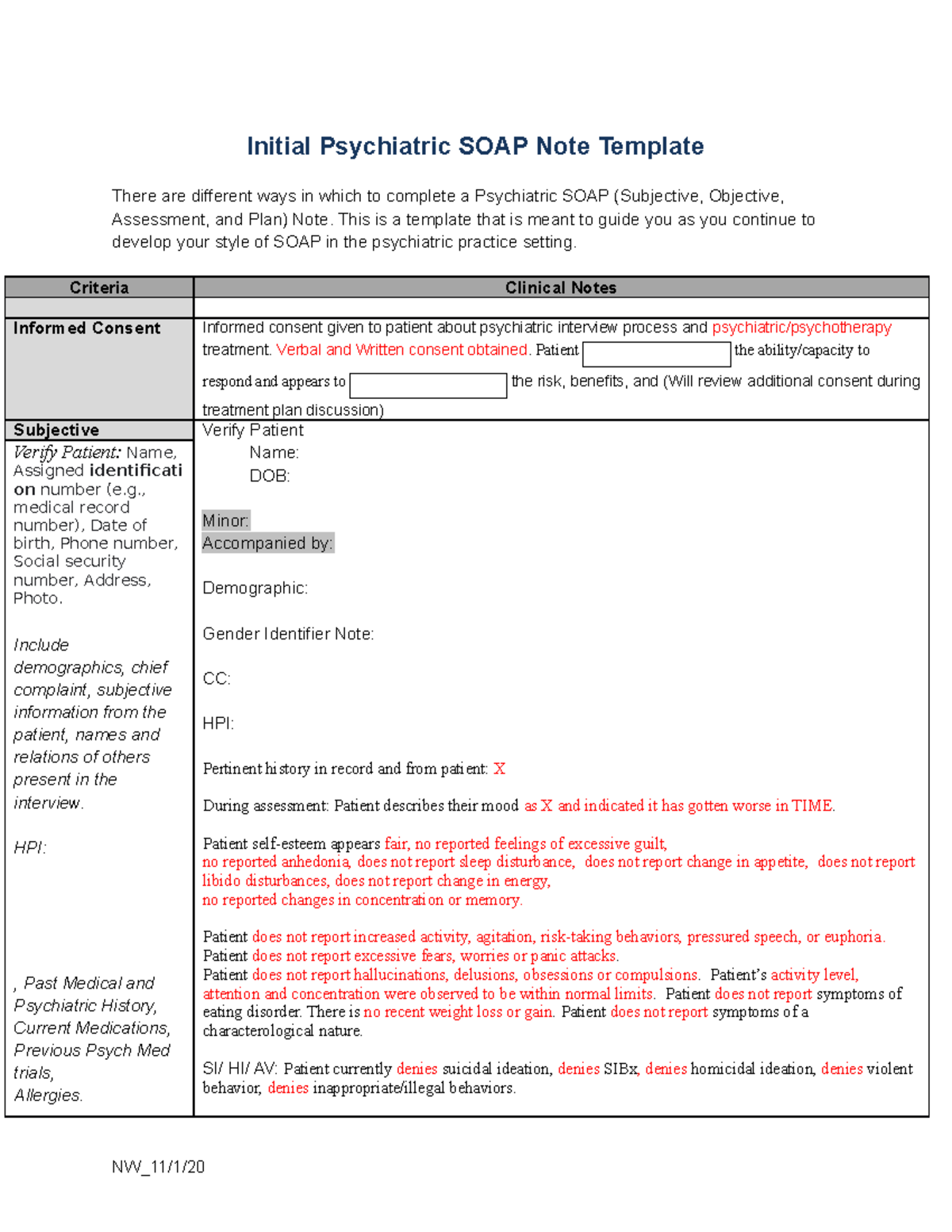
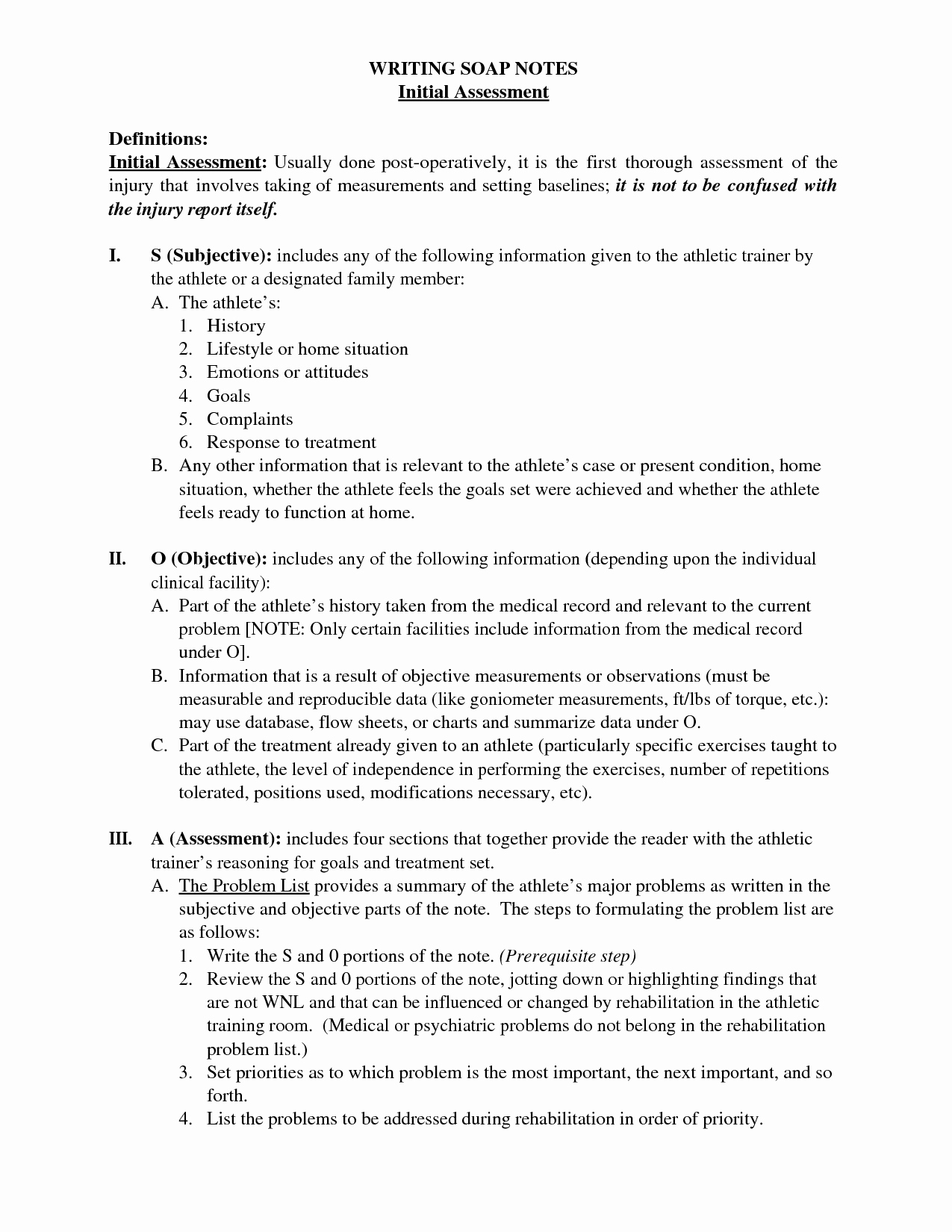
Psychiatry Soap Note Template - Learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. Currently receiving out p atient mental health treatment bipolar disorder. The soap notes format is essentially a templated approach to documenting patient interactions and assessing their condition in a structured and repeatable way. Web mental health professionals can use soap note templates for anxiety and depression for example to ensure they are effectively documenting the essential information needed for effective treatment planning and collaboration with other providers. Please document if the condition has worsened, improved, resolved over the past weeks, months or years. History of present illness provide a focused description of symptoms. [text name=patientname default=] patient date of birth: One or more chronic illnesses with severe exacerbation, progression, or side effects of treatment the following interventions were ordered/recommended this appointment: Web in psychiatry, we often document a patient’s current condition and progress in treatment with soap notes. Web high (99215)= psychiatric illness with potential threat to self or others, drug therapy requiring intensive monitoring for toxicity; Web pmhnp long note. Learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. Chief complaint a statement in “quotes” describing what the patient presents for today: [text name=dob default=] medical record number: Download template download example pdf. [text name=medicalrecord default=] provider name: Web past psychiatric history : Web soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice. Gait and station / muscle strength and tone: Web in this post, we will review what soap notes are, how to write a. 0.55 approximately 42 views in the last month. This guide provides a thorough overview of soap notes, their purpose, and essential elements tailored for pmhnps. Chief complaint a statement in “quotes” describing what the patient presents for today: Web soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in. Web here’s how to write soap notes. Depressive symptoms have improved but he still feels down at times. This is a template that is meant to guide you as you continue to develop your style of soap in the psychiatric practice setting. 5+ psychiatric soap note examples; However, the structure of the information and its Approximately 49 views in the last month. The soap (subjective, objective, assessment, and plan) format is commonly used in medical documentation and includes information about the patient's symptoms, a mental status examination, an assessment of the patient's. As you know, soap stands for the areas of documentation that are considered vital components in order to achieve our goals with treatment.. Web this is a template that is meant to guide you as you continue to develop your style of soap in the psychiatric practice setting. History of present illness provide a focused description of symptoms. Calculator, csv ready, mental status exam. What is the benefit of using. Web here’s how to write soap notes. Check out these soap notes for psychiatry templates to improve your clinical notes, productivity, and mental health outcomes. Web soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice. Web soap notes, are a specific format used for writing a progress note.this packet of. Web free soap notes for psychiatry template. This is a template that is meant to guide you as you continue to develop your style of soap in the psychiatric practice setting. Please document if the condition has worsened, improved, resolved over the past weeks, months or years. Download our comprehensive soap note pdf template for mental health professionals and other. Nw_11/1/20 criteria clinical notes informed consent informed consent given to patient about psychiatric interview process and psychiatric/psychotherapy treatment. [text name=medicalrecord default=] provider name: Web initial psychiatric soap note template there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Gait and station / muscle strength and tone: Jan has been hospitalized on a. Counselors, social workers, psychologists etc. Web free soap notes for psychiatry template. 5+ psychiatric soap note examples; Soap note for medical practitioners (care cloud, n.d.): Currently receiving out p atient mental health treatment bipolar disorder. Web mental status examination. Calculator, csv ready, mental status exam. History of present illness provide a focused description of symptoms. In psychiatry, some of the specifics may be unique; Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Web this is a template that is meant to guide you as you continue to develop your style of soap in the psychiatric practice setting. Web comprehensive psychiatric examination. One or more chronic illnesses with severe exacerbation, progression, or side effects of treatment the following interventions were ordered/recommended this appointment: Web by taking typed or handwritten notes according to each category of soap, you can better track and organise your patient care in a standardised manner. This is a template that is meant to guide you as you continue to develop your style of soap in the psychiatric practice setting. Soap note for medical practitioners (care cloud, n.d.): Nw_11/1/20 criteria clinical notes informed consent informed consent given to patient about psychiatric interview process and psychiatric/psychotherapy treatment. Counselors, social workers, psychologists etc. The soap (subjective, objective, assessment, and plan) format is commonly used in medical documentation and includes information about the patient's symptoms, a mental status examination, an assessment of the patient's. Web in psychiatry, we often document a patient’s current condition and progress in treatment with soap notes. Web comprehensive psychiatric soap notedate: Web soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice. Download template download example pdf. The soap notes format is essentially a templated approach to documenting patient interactions and assessing their condition in a structured and repeatable way. Please document if the condition has worsened, improved, resolved over the past weeks, months or years.FREE 9+ Sample SOAP Note Templates in PDF MS Word
Psychiatric Soap Note Example
Tips for Writing Better Mental Health SOAP Notes [Updated 2021]
Psychiatry Soap Note Template
Psychiatry Note Template
Psychiatric Soap Note Template
NU646 Initial Psychiatric SOAP Note Template Initial Psychiatric SOAP
Psychiatry Soap Note Template
Psychiatric soap Note Example Peterainsworth
Pt soap note example. 15 SOAP note examples and templates (2023 Update
Related Post: